Head & Neck Cancer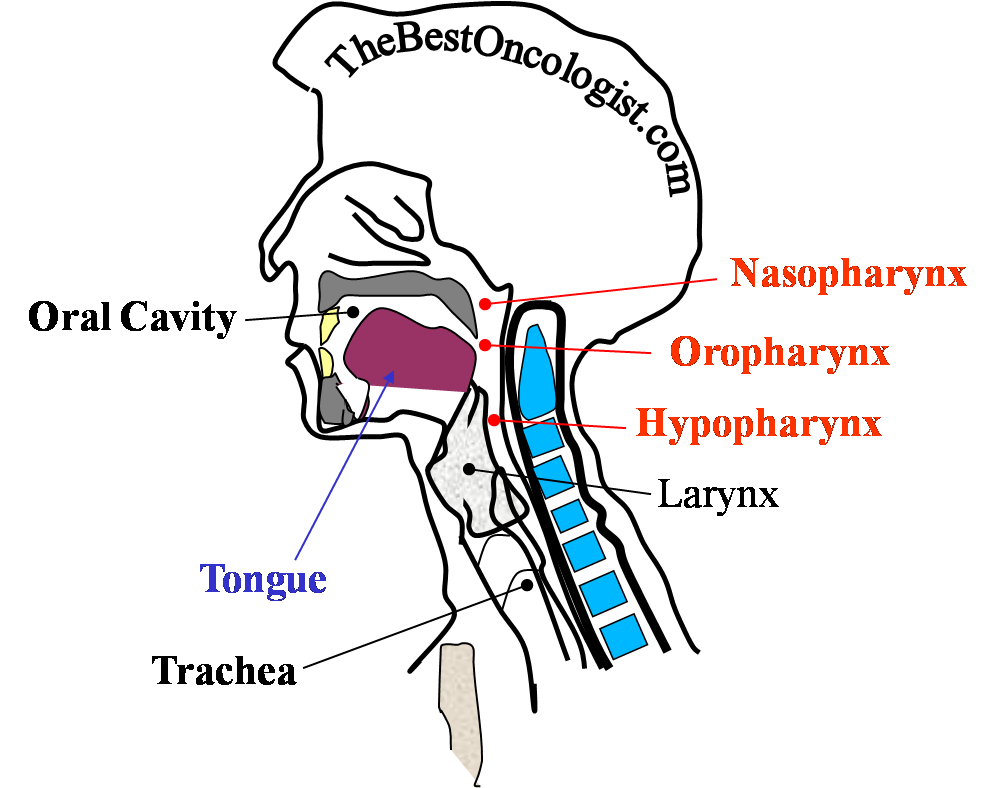
Surgical resection
Radiation therapy
Chemotherapy
Combined chemo-radiation
Head & Neck Cancer
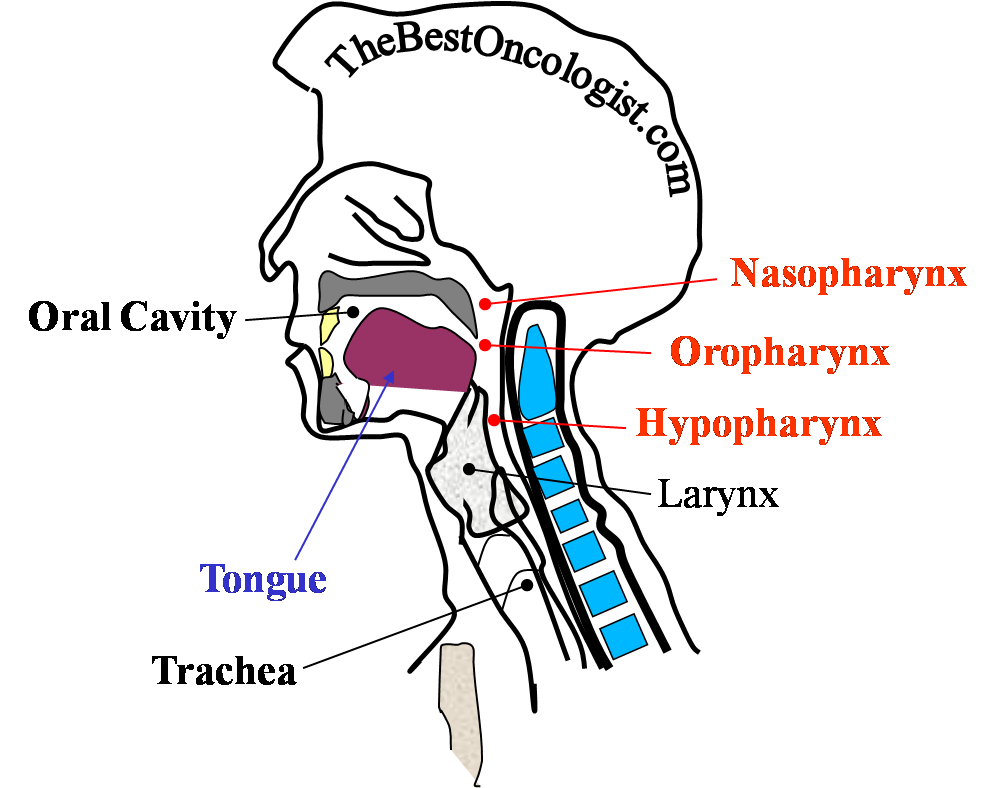
Head & Neck (H&N) cancer represents about 3-6 %
of the newly diagnosed cancers. Each year more than 650000 new
patients are diagnosed world-wide. This disease is more prevalent
among men than women (2:1 ratio).
Risk factors are mainly Smoking and Alcohol consumption; when
combined, the risk markedly increases. Higher incidence of H&N
cancer was also observed after radiation exposure (Chernobyl). Ultra violet light is correlated
with some of H&N cancers (lip cancer).
Squamous Cell Carcinoma is the most prevalent
entity and occurs in more than 90% of cases.
The most important parameter for treatment of
H&N cancer is the stage of the disease. Localized disease without
lymph nodes involvement or distant spread yields the most favorable
prognosis. Distant spread occurs most commonly to lungs.
Several steps should be performed for
diagnosis of H&N cancer:
- Careful history taking from the patient by an experienced
physician. Patients may be asymptomatic, but complaints such as
difficulty in swallowing (dysphagia), painful swallowing (odynophagia),
nasal obstruction or
bleeding (epistaxis), hearing impairment and changes in
the patient’s voice may be elicited. These symptoms can direct
the clinician to the problem site.
- Careful physical examination, including ear, nose and throat
inspection. Special attention should be given to discover and
document any enlarged lymph nodes. Neurological examination
including cranial nerves testing should be performed.
- Laboratory tests. These tests should include a complete
blood cell count, serum electrolytes (including calcium), and
liver and kidney function tests.
- Radiological evaluation should include contrast enhanced
computerized tomography of the head and neck, chest radiograph/
chest computerized tomography. Magnetic resonance imaging should
be spared to selected patients; bone scan should be performed if
there is clinical or laboratory suspicion of bone metastasis
(increased calcium levels, bone pain…) or if lymph nodes
enlargement exist; positron emission tomography should be
considered for detection of metastatic disease. The decision
regarding the diagnostic modalities should be determined
according to the clinical judgment of the treating oncologist.
- Tissue biopsy should be obtained in order to make the final
diagnosis. Biopsies are usually obtained from the most easily
approached disease site.
The most used staging system is that of the
American Joint Committee on Cancer (cancer staging manual 6th
edition, NY, Springer –Verlag, 2002).
The decision regarding the treatment of H&N
cancer should be tailored to every patient, and should be designed
by a multidisciplinary team of physicians that includes surgeons,
ENT specialists, radiation oncologist and clinical oncologist. The
treatment modalities are:
Surgical resection. Surgical resection
is considered in patients with H&N cancer who suffer from squamous
cell carcinoma and localized disease.
Radiation therapy. Play a pivotal role
in the treatment of patients with H&N cancer. Mostly, 6-7 weeks (5
days/week) of radiation therapy (2 Gy/d; 60-70 Gy/course) is
administered. Several groups suggest applying radiation therapy
twice/ three times daily and thus shortening the time of treatment
and probably increasing its efficiency; these regimens are currently
experimental.
Chemotherapy. Chemotherapy is given to
locally advanced or metastatic disease. Combination chemotherapy is
superior to single agent treatment. One drug should be platinum
based (cisplatin or carboplatin). Neoadjuvant chemotherapy
(administered before performing surgical resection) resulted in more
successful organ preservation (e.g. laryngeal cancer).
Combined chemo-radiation. Radiation may
be combined with intravenous weekly cisplatin, or with weekly
carboplatin and paclitaxel. The later combination is used if a
contraindication to cisplatin exists (hearing loss, neuropathy,
kidney disease…). Chemo-radiation is used for curative intent, as
primary or adjuvant (after
performing surgical resection) treatment, and give superior
results than treatment with chemotherapy alone. Adjuvant
Chemo-radiation is recommended for locally advanced head and neck
cancer.
-
Specenier PM, Vermorken JB.
Neoadjuvant chemotherapy in head and neck cancer: Should it be
revisited?
Cancer Lett. 2007; 256(2):166-77.
Read This Article
-
Bernier J.
Head
and neck oncology: what the past decade has taught us.
Expert Rev Anticancer Ther. 2006; 6(9):1133-6.
Read This Article
-
Bernier J, Domenge C, Ozsahin M, Matuszewska K, Lefebvre JL,
Greiner RH, Giralt J, Maingon P, Rolland F, Bolla M, Cognetti F,
Bourhis J, Kirkpatrick A, van Glabbeke M; European Organization
for Research and Treatment of Cancer Trial 22931.
Postoperative irradiation with or
without concomitant chemotherapy for locally advanced head and
neck cancer.
N Engl J Med.
2004; 350(19):1945-52.
Read This Article
-
Huguenin P, Beer KT, Allal A, Rufibach K, Friedli C, Davis JB,
Pestalozzi B, Schmid S, Thoni A, Ozsahin M, Bernier J, Topfer M,
Kann R, Meier UR, Thum P, Bieri S, Notter M, Lombriser N,
Glanzmann C.
Concomitant cisplatin
significantly improves locoregional control in advanced head and
neck cancers treated with hyperfractionated radiotherapy.
J Clin
Oncol. 2004; 22(23):4665-73.
Read This Article
-
Cooper JS, Pajak TF, Forastiere AA, Jacobs J, Campbell BH,
Saxman SB, Kish JA, Kim HE, Cmelak AJ, Rotman M, Machtay M,
Ensley JF, Chao KS, Schultz CJ, Lee N, Fu KK;
Radiation Therapy Oncology Group 9501/Intergroup.
Postoperative concurrent radiotherapy and chemotherapy for
high-risk squamous-cell carcinoma of the head and neck.
N Engl
J
Med.
2004; 350(19):1937-44.
Read This Article
-
Juweid ME, Cheson BD.
Positron-emission tomography and assessment of cancer therapy.
N Engl
J
Med.
2006; 354(5):496-507.
Read This Article
-
Buck
G, Huguenin P,
Stoeckli SJ. Efficacy of neck
treatment in patients with head and neck squamous cell
carcinoma.
Head Neck. 2007; DOI
10.1002/hed.20657.
Read This Article
-
Agarwala S, Cano E, Heron D, Johnson J, Myers E, Sandulache V,
Bahri S, Ferris R, Wang Y, Argiris A.
Long-term outcomes with concurrent carboplatin, paclitaxel and
radiation therapy for locally advanced, inoperable head and neck
cancer.
Ann
Oncol. 2007; 18(7):1224-1229.
Read This Article
-
Hitt R, Lopez-Pousa A, Martinez-Trufero J, Escrig V, Carles J,
Rizo A, Isla D, Vega ME, Marti JL, Lobo F, Pastor P, Valenti V,
Belon J, Sanchez MA, Chaib C, Pallares C, Anton A, Cervantes A,
Paz-Ares L, Cortes-Funes H. Phase III
study comparing cisplatin plus fluorouracil to paclitaxel,
cisplatin, and fluorouracil induction chemotherapy followed by
chemoradiotherapy in locally advanced head and neck cancer.J
Clin Oncol. 2005; 23(34):8636-45.
Read This Article
-
Adelstein DJ, Leblanc M.
Does induction chemotherapy have a role in the management of
locoregionally advanced squamous cell head and neck cancer?
J
Clin Oncol. 2006; 24(17):2624-8.
Read This Article
-
Zorat PL, Paccagnella A, Cavaniglia G, Loreggian L, Gava A,
Mione CA, Boldrin F, Marchiori C, Lunghi F, Fede A, Bordin A, Da
Mosto MC, Sileni VC, Orlando A, Jirillo A, Tomio L, Pappagallo
GL, Ghi MG.
Randomized phase III trial of
neoadjuvant chemotherapy in head and neck cancer: 10-year
follow-up.
J Natl Cancer Inst. 2004; 96(22):1714-7.
Read This Article
|